GET STARTED
The journey to a healthier and happier life begins with simple steps. Here are seven easy ways that you can help yourself and spread awareness about Polycystic Ovary Syndrome. Discover the various ways that you can stay connected with PCOS Challenge and access the content that is of greatest interest to you.


PCOS SUPPORT
PCOS Challenge provides support for women with PCOS through television and radio programming, educational workshops and online and offline support networks. Our programs help women overcome their struggles with infertility, weight gain, anxiety and depression and reduce their risk for life-threatening related diseases.


DONATE
Millions of women with Polycystic Ovary Syndrome are going undiagnosed, untreated and unsupported. Help make PCOS a public health priority. Nearly two-thirds of our annual budget comes from individual donors like you. Every gift and every dollar amount makes a difference. Please Donate Now.


PCOS RADIO
Sasha Ottey, Founder and Executive Director of PCOS Challenge, Inc., hosts the PCOS Challenge® radio show, designed to inform people about PCOS and related conditions. The popular radio show features interviews with renowned PCOS experts, New York Times best-selling authors and real life stories from women with PCOS.


PCOS GRANTS
PCOS Challenge offers the PCOS Challenge Family Building Grant for individuals with PCOS struggling with infertility, which includes a free IVF cycle. PCOS Challenge also offers the PCOS Confidence Grant to help individuals with hair and skin issues related to PCOS, which includes a grant up to $500 to help with the cost of related hair and skin treatments.


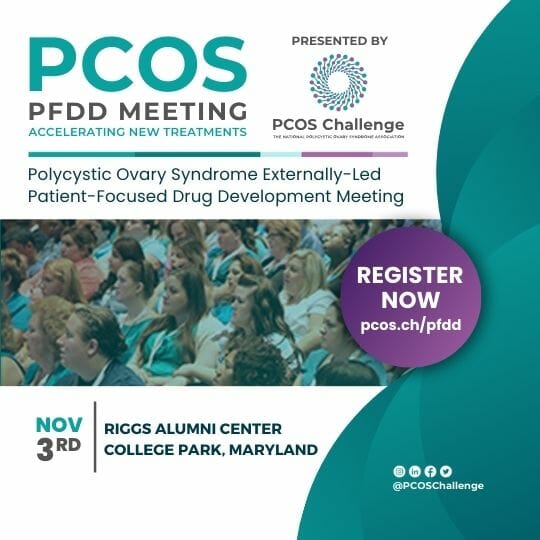
PCOS EVENTS
The PCOS Awareness Symposia, presented by PCOS Challenge are the largest series of events globally dedicated to Polycystic Ovary Syndrome. The symposia bring together clinicians, researchers, hundreds of women with PCOS and their supporters for a day of sharing experiences, insights and the latest updates about the condition.